People who are at highest risk of catching the monkeypox virus will soon be offered a vaccine in an effort to reduce transmission.
The UK’s Health Security Agency (UKHSA) has revealed that some men who have sex with men will soon be offered the Imvanex jab – originally designed to treat smallpox – to curb the largest recent outbreak outside of Africa.
Advertisement
Here’s why.
Who is at high risk and why?
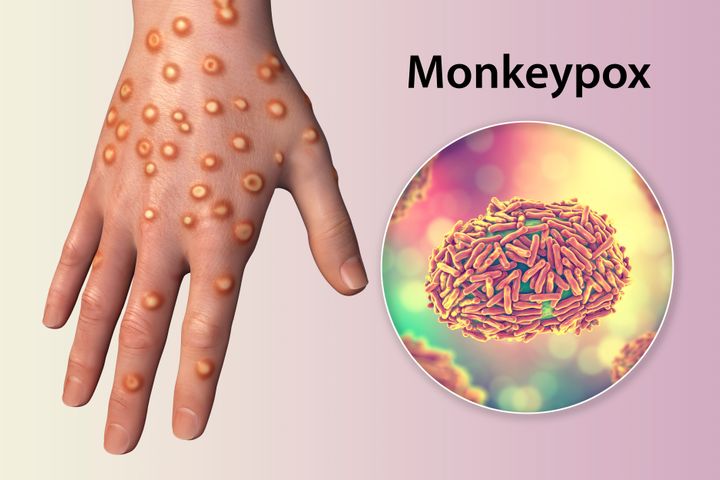
Monkeypox is not sexually transmitted, but can be passed on through close contact which is why it has become associated with sex.
The World Health Organisation (WHO) believes that the outbreak stemmed from sexual activity by men at raves in Spain and Belgium.
More than 99% of the current 793 reported UK cases are among men, most of whom identify as gay or bisexual.
Anyone – regardless of sexual orientation – is at risk of contracting the virus if they are in close contact with someone infected with monkeypox, or infected clothing or bedsheets.
Advertisement
But, men who have sex with men and who have multiple partners are considered at the highest risk – this includes those who take part in group sex, or go to venues where sex occurs on the premises – due to the origins of this particular outbreak.
The agency said data suggests there are higher levels of transmission “within, but not exclusive to, the sexual networks of gay, bisexual and other men who have sex with men”.
UKHSA’s head of immunisation Dr Mary Ramsay said: “By expanding the vaccine offer to those at higher risk, we hope to break chains of transmission and help contain the outbreak.”
Is this the first group to be offered the vaccine?
No – vaccines were offered to health workers who look after monkeypox patients as well as cleaners disinfecting areas which may have been exposed to the virus.
Close contacts of confirmed cases were also offered the vaccine.
NHS England will soon provide more details about how those who are eligible can receive a jab, although people are advised not to approach the NHS until contacted.
Advertisement
Vaccines have never been used in Africa to impact monkeypox, even though it is endemic in some countries.
It’s also worth noting that this vaccine is not designed specifically for monkeypox. Although Imvanex was used to eradicate smallpox worldwide, it has been found to be 85% effective against this current virus.
KATERYNA KON/SCIENCE PHOTO LIBRARY via Getty Images
Does this news mean there’s cause for concern?
Well, it’s unclear at the moment.
No deaths outside of Africa have yet been reported from this outbreak, although confirmed cases have suffered from fever, swollen glands and a rash which develops into fluid-filled lumps.
There are currently 793 cases in the UK out of more than 2,100 cases around the world – far lower numbers compared to when the Covid vaccine rollout first began.
Advertisement
However, the Joint Committee on Vaccinations and Immunisations (JCVI) supported the decision to start handing out the smallpox vaccine. This panel advised the government to start its vaccination programme for Covid last year.
The WHO has described the outbreak outside of the continent as “unusual and concerning”, and is considering declaring it a global emergency.
Dr Ramsay warned: “Although most cases are mild, severe illness can occur in some people, so it is important we use the available vaccine to target groups where spread is ongoing.”
Professor Paul Hunter from University of East Anglia’s school of medicine also told Sky News that vaccination was “the right thing to do”.
He added: “What we have seen with monkeypox is a significant and continuing increase of the second wave despite control measures having been in place for a few weeks.
Advertisement
“So it is certainly looking like the current strategy of ring vaccination is not working.
“This is probably down to difficulties in identifying cases and their contacts rapidly enough, possibly due to stigma.”
He suggested that “we should be ready to start offering the vaccine to female sex workers” as well, because the virus does not discriminate by sexual orientation or sex.
The WHO has also called for the virus to be renamed after experts appealed for a “non-discriminatory” alternative.
If you think you have monkeypox…
You’ll have to do a PCR test similar to the Covid test. For monkeypox, it involves three swabs, two for the skin, and a throat swab.
You are still allowed to travel on public transport if you suspect you’ve caught the virus, but wear a mask and cover any lesions.
If you need to isolate, do not share a bathroom if you can avoid it and isolate in one room. Make sure not to share bedding or towels, avoid contact with your pets and have no sexual contact.
Try to avoid other communal spaces, too, such as the kitchen.