A colonoscopy brings with it a sense of uncertainty – not helped by gut health and bowel movements still being stigmatised by society.
I have struggled with my bowels since my teens. Diarrhoea and urgency made my life miserable, but I became more concerned when I also started passing blood.
My GP had previously given me a diagnosis of irritable bowel syndrome (IBS), although everything I read about it suggested bleeding was not usually a symptom. A fatigue like no other began to consume me, too, along with aches in my elbows and wrists. After further tests and a hospital admission (and many years), I was referred for a colonoscopy.
Although I knew the word, I didn’t know what the procedure entailed.
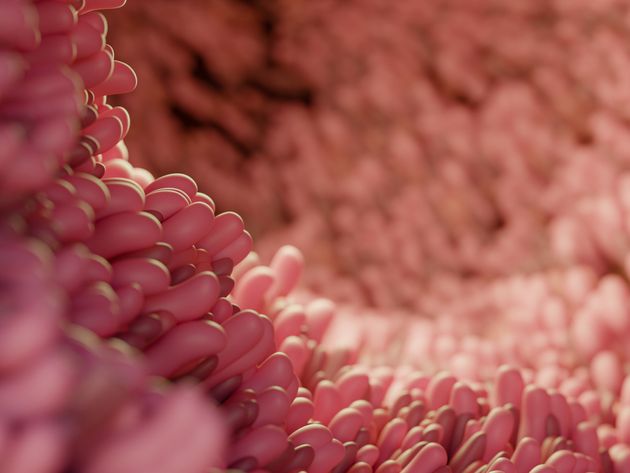
The leaflet given to me by the hospital was clear but clinical and told me the basics – that a colonoscope – a camera on a long, thin tube – is used to view the rectum and bowel. The colonoscope is inserted into the anus and shows your lower digestive tract on a screen. Images alone may be enough to make a diagnosis, but biopsies are sometimes also taken.
The idea of someone pushing a tube up my bum didn’t fill me with joy but I knew it was a vital step on the road to finding out what was wrong with me.
A week or so before my appointment a package arrived from the gastroenterology unit. As well as another copy of the leaflet I’d been given previously, there was a questionnaire to complete and return, along with sachets of a powder called Moviprep. A printout itinerary was also included, telling me how to prepare for the colonoscopy.
To see the bowel clearly, it needs to be completely empty which involves a period of fasting. This is also where the Moviprep came in. Instructions told me that the night before the colonoscopy I was to mix a sachet with two litres of water and then slowly drink the concoction.
The hazy mixture made me gag – it tasted of lemon and dust – but I knew this was the best way to get clear images. Finishing the jug felt like a win, but this was only the halfway point. A second jug had to be drank and this was infinitely harder as the Moviprep was taking effect and I was rushing to the bathroom regularly.
My stomach was bloating from drinking such large volumes. It wasn’t a fun experience, but I finished the second two litres, then spent the rest of the evening reading a book on the toilet before heading to bed.
Surprisingly, I slept until the rude awakening from my alarm clock signalled it was time for more Moviprep. Drinking another four litres on an empty stomach was a challenge but the trips to the bathroom that followed proved my bowels were clear – all I was passing was a slightly yellow-tinged liquid.
When I arrived at the hospital a nurse ran through the questionnaire I’d completed, asked if I’d completed the Moviprep and took my blood pressure and pulse rate. Satisfied that I met the criteria, he gave me the paperwork to sign to agree that I was happy for the procedure to go ahead. Once complete, I was given a hospital gown and paper pants to wear and told to wait for my slot.
By this point I was impatient, edgy, and hungry. Thankfully, it wasn’t long until a healthcare assistant showed me to the colonoscopy suite, instructing me to lie on my left-hand side and telling me how to use the gas and air (it is also possible to be sedated for a colonoscopy if you have someone to take you home).
The doctor who was carrying out the procedure showed me the colonoscope then a gel lubricant was applied, and, after a few puffs of Entonox, we were ready to go. The insertion was uncomfortable but not painful and I focused on the screen – after all, how often do you get to see your insides?
Being honest, I was light-headed throughout. My stomach was swelling, a result of the air used to help the doctor get clear images. The healthcare assistant was talking to me as I watched the images of the colonoscope moving through my bowel.
There were two points where it hurt, which the doctor explained was where my bowel twisted. I was given the option of stopping the procedure, but I persevered, not wanting to have to go through the entire process again. Thankfully, they were able to get the whole way around my bowel by moving me onto my stomach, although this did make me break wind! I immediately felt more comfortable, and they were able to take biopsies from various parts of my bowel.
After about 45 minutes it was all over and I was wheeled to the recovery area to rest, get changed and have an all-important cup of tea and a sandwich. I was then given a discharge form telling me when to expect the results and any warning signs to look out for before being sent home.
Two weeks later the results were in – I was officially diagnosed with Crohn’s Disease. Since then, I have had more colonoscopies and, although not pleasant, I know it is an important part of my healthcare routine.
If you are called for a colonoscopy, try not to be nervous. It is a common procedure, with around 900,000 conducted each year in the UK.